Do you need care at Mater Hospital Brisbane's Emergency Department?
Treatment costs
Effective 1 July 2025. Costs are subject to change. You will be requested to pay these fees prior to treatment
Emergency department
The treatment cost is based on your triage category:
Triage category | Cost |
Category 1 | $1,536.30 |
Category 2 | $1,294.40 |
Category 3 | $972.65 |
Category 4 | $623.80 |
Category 5 | $396.80 |
Additional costs:
Additional services may be billed separately by external providers.
Please contact these providers directly for quotes.
May include:
- Diagnostic imaging (Medicare Benefits Schedule fee)
- Pathology services ($124.25 per request)
- Pharmaceuticals (full cost)
- Prosthetics/medical aids/appliances admitted services fees (see below)
- Inter hospital ambulance transport
Admitted services
Accommodation fee in a general medical ward:
- Overnight ($2,595.90 per night)
- Same day ($2,193.70)
Wards providing specialised care charge higher fees:
Ward | Cost per day |
Intensive Care Unit | $6,536.00 |
Coronary Care Unit | $4,372.35 |
Rehabilitation | $1,364.00 |
Renal Dialysis | $1,219.90 |
Special Care Nursery/Neonatal Intensive Care | $4,204.80 |
Neonatal Intensive Care older than 9 days | $6,536.00 |
You may incur costs from external service providers. Please contact them directly for estimated fees.
These may include:
- Radiology (MBS fee)
- Pharmaceuticals
- Prosthetics, medical aids, appliances
- Inter-hospital ambulance transport
Frequently asked questions
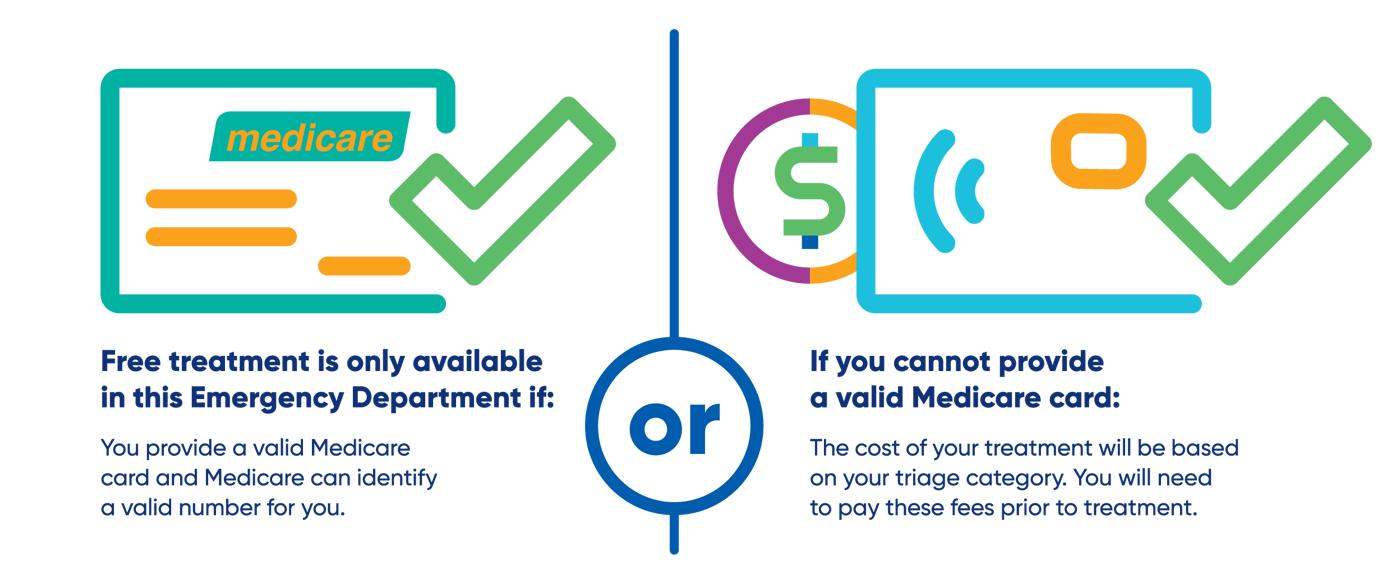
I have a Medicare card but did not bring it today
You must bring your Medicare card to every hospital visit. If you do not have your card with you, we will attempt to verify your details using Medicare Online.
If we are unable to verify your Medicare details and you do not have a valid Medicare number on file, an invoice will be issued for payment on the day. If you provide your Medicare number after treatment and we can validate it, we will refund your payment.
I have been admitted. What can I expect?
On admission to hospital you will be required to pay for the triage service of emergency and any radiology costs incurred. You will be provided with an informed financial consent for which is an estimate of the costs associated with your admission at that time. This estimate will be updated throughout your admission as the actual costs for your care become clearer.
You will be asked to pay an upfront admission fee of three nights plus theatre charges prior to admission. If you have an insurance policy, you will be able to submit the claim to the insurer post discharge for reimbursement.
Medicare Ineligible patients will be charged for tissue and blood products at full cost.
The following Medicare ineligible patients may not need to pay
Asylum seekers or refugees referred from the Mater Refugee Complex Care Clinic, Tuberculosis patients, or those receiving care under a Health Directive Service.
I was in a work accident. Do I need to pay?
If you are Medicare ineligible and do not have an approved workers’ compensation claim, you must pay for treatment. If your claim is later approved, we will refund money paid on verification of cover.
Do I pay if I was in a motor vehicle accident?
If you are Medicare ineligible, and do not have an approved insurance claim or cannot provide all the accident details including the driver at fault required to qualify for motor accident funding, you must pay for treatment. If it is later found that you have an approved insurance claim or qualify for motor accident funding, we will refund money paid on verification of cover.
What is a Reciprocal Healthcare Agreement?
Australia has Reciprocal Healthcare Agreements (RHCA) with eleven countries. The agreements provide visitors to Australia with subsidised medical treatment.
Eligible Countries (as at 1 February 2024):
- Belgium
- Finland
- Italy (eligibility limited to six months from date of arrival)
- Malta (eligibility limited to six months from date of arrival)
- Netherlands
- New Zealand (public hospital care and PBS medicines only, not MBS services)
- Norway
- Ireland (public hospital care and PBS medicines only, not MBS services)
- Slovenia
- Sweden
- United Kingdom
Eligible patients from these countries need to enrol in Medicare to access Medicare Benefit Scheme services (MBS). Once enrolled they will be issued with a yellow Medicare card which you can use at emergency and outpatient attendances.
Visitors from New Zealand and Ireland do not need to enrol in Medicare to access public hospital services and PBS medicines under the Reciprocal Health Care Agreements. They are not eligible for MBS services unless they hold a green Medicare card.
Specifically, if you are visiting Australia from a country with an RHCA, you generally need to enrol in Medicare to utilise the agreement’s benefits, including access to public hospital services.
I am from a country with a reciprocal healthcare agreement. What do I need to do?
To show that you qualify for treatment under a reciprocal healthcare agreement, we need to view your Medicare Reciprocal card. If you are from New Zealand or The Republic of Ireland, you will need to provide copies of both your:
- Current passport
- Visa grant notice
We will ask for these documents at every presentation.
If you do not bring these, you must acknowledge the cost of treatment at Medicare ineligible rates and pay prior to your treatment.
If you later provide the copies of these documents as evidence you qualify for treatment under the agreements, we will refund money paid.
Who can I speak with regarding my bill?
If you have any questions about your bill, please contact our Business Services team on 07 3163 1515.
What happens with fees if I have emergency care and then need planned treatment?
- Your initial emergency care is billed according to your Medicare eligibility.
- If you need to return for planned, follow up, or elective care after your ED visit, you will be treated as a private patient in a public hospital.
- Private patient charges will apply for consultations, procedures, tests, and anaesthetics (MBS rates).
- Additional costs may apply, such as operating theatre fees, pharmaceuticals, medical aids, and ambulance transfers.