Corneal transplantation is a major commitment, which requires lifelong care by the patient to maintain the graft and preserve vision.
What is the cornea?
The cornea is the clear, dome-shaped tissue covering the front of the eye. It is about the size of a dime and the thickness of a credit card. The cornea is kept moist and nourished by a thin layer of tears. It is kept smooth by the blinking of the eyelids. If the cornea becomes distorted in shape, scarred, or hazy (opaque) from disease or injury, the light rays passing through it are distorted and the vision is reduced. In some cases, a corneal transplant may be necessary to replace the diseased or injured cornea with a healthy, clear cornea to restore good vision.
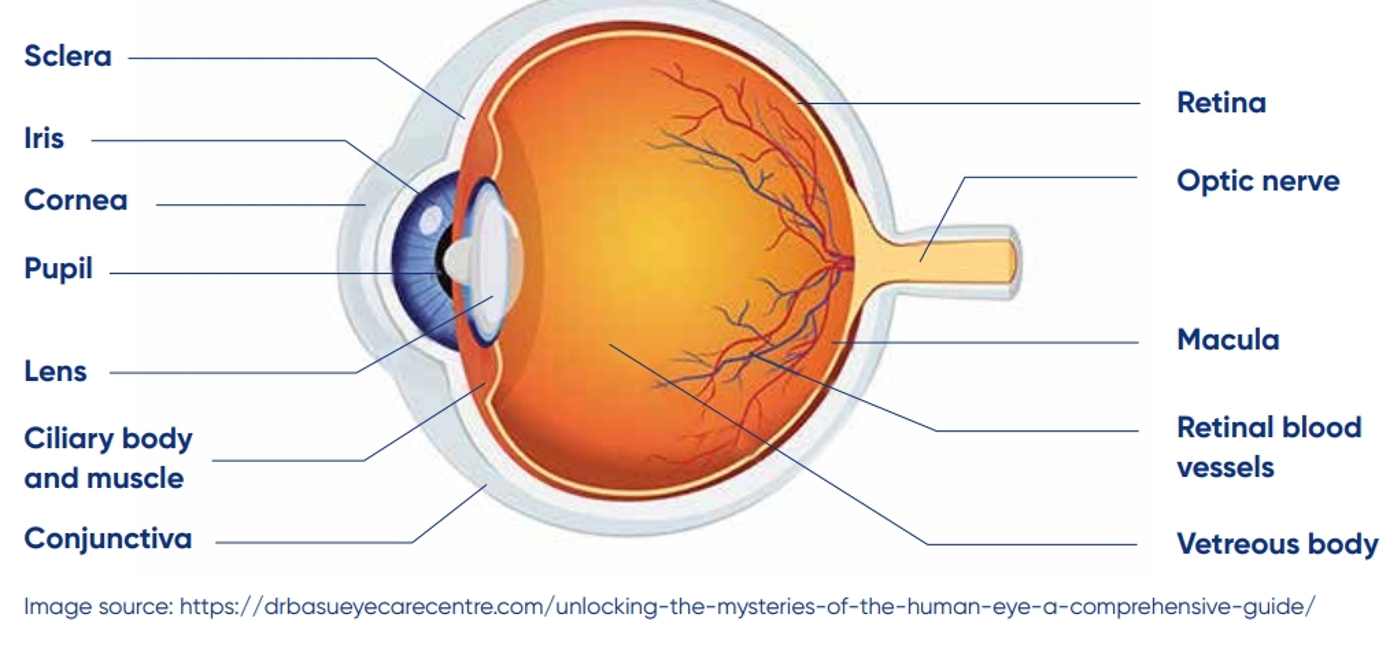
The human eye
What is corneal transplant surgery?
In corneal transplant surgery, the scarred or damaged cornea is removed and replaced by a human donor cornea called a graft. Your eye is the recipient eye because it receives the graft. The other person’s cornea is the donor cornea or donor tissue because the cornea is being donated or given to you. Depending on the disease, sometimes all layers of the cornea are replaced, other times only part of the cornea layers are transplanted.
The donor cornea
An eye bank provides the donor tissue for corneal transplant surgery. The corneas are obtained from deceased individuals who arranged for donation prior to their death or whose families gave permission. The organ you receive is precious and should be treated with due respect.
The surgery
Most eye surgeries are performed under local anaesthetic with some sedation. Your doctor will select the type of anaesthesia based on the kind of corneal transplant surgery you are having as well as your medical history. You can usually go home the same day as your operation, but you will need to attend an appointment in the eye clinic the next day.
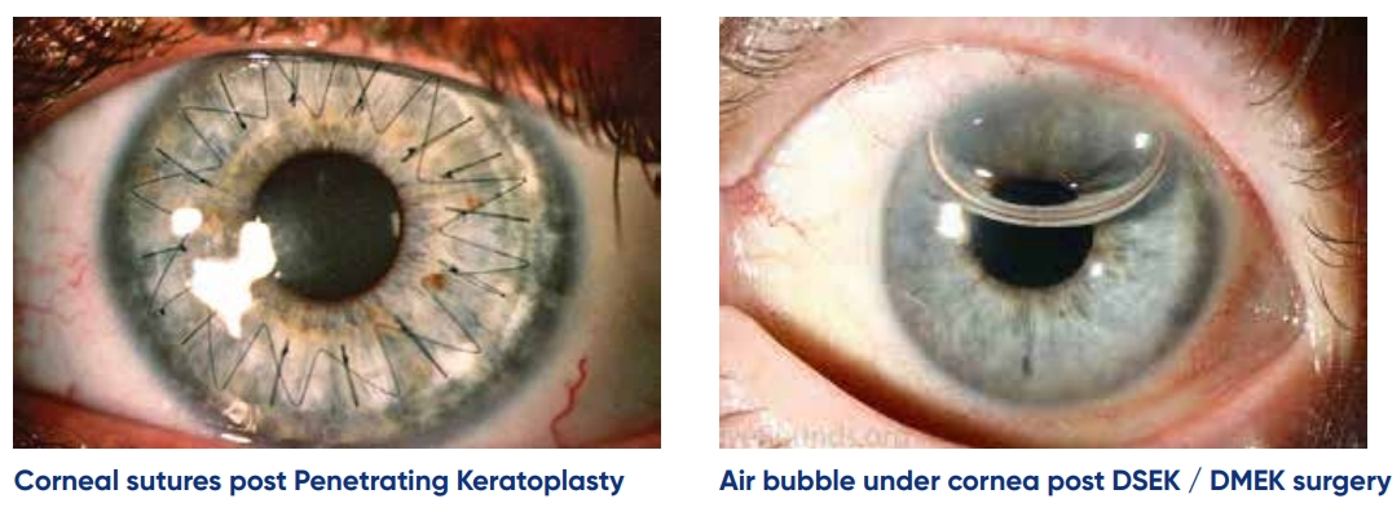
Image sources - https://keratoconusgb.com/what-is-a-corneal-graft-or-transplant/ and https://eyerounds.org/tutorials/Cornea-Transplant-Intro/5-DMEK.htm
Penetrating keratoplasty (PK) / DALK – “Full thickness transplant / partial thickness transplant”
A central circle of your diseased cornea is removed and replaced by the clear donor cornea. It is stitched into place with numerous very fine sutures which are smaller in diameter than human hair. These stitches do not dissolve and remain in place for at least a year, they can be removed in clinic when appropriate. A DALK preserves the most inner lining of your natural cornea, whereas a PJ replaces all layers of the cornea. A DALK is stronger and has less risk of rejection but is not suitable in all patients. Even when a DALK is the intended operation, sometimes attempts at a DALK are unsuccessful and a PK is performed instead at the time of surgery. Your vision will not be as good as it can until all stitched are removed and glasses are obtained. Although you may see a bit better early on, the road to improved vision is long, potentially 1-2 years before your vision is optimised.
DMEK / DSEK – “Inner layer transplant”
In some situations, your surgeon may transplant only the most inner lining of your cornea. Here a gas bubble will be used to help it stick onto the inside surface of your cornea. If a gas bubble is inserted in your eye you may have to follow certain protocols for positioning after surgery (lying on your back), and you will be restricted from flying in the weeks/months after your operation.
Graft rejection
There is always a possibility that the body will reject the graft. This is like an “allergic” reaction of the body against the donor cornea. It can occur any time after the surgery. There is a good chance this can be treated successfully if you act immediately. There are four danger signs you must know. If any of these occur and last for more than 12 hours, you should call the hospital or present to your local optometrist or emergency department – even if it is a weekend or holiday. To remember the signs of graft rejection, remember the letters:
RSVP
Redness
Sensitivity
Vision changes
Pain
Make a habit of checking your eye every day. Check your vision at about the same time and in the same lighting each day, perhaps at the same time as another routine activity such as brushing your teeth.
If at any time you experience the following symptoms after your surgery, you should call the Mater Eye Clinic on 07 3163 5694, or out of hours, the Mater Hospital on 07 3163 8111, 07 3098 8111 or present to your closest emergency department / eye clinic / local optometrist.
Redness
For a few weeks after surgery, your eye may be red. Increasing redness may be a sign of graft rejection. Check the redness of your eye by looking into a mirror and pulling down the lower lid. Look carefully at the white of the eye, especially in the area next to the cornea.
Sensitivity to light
Bright lights may seem irritating to your eye after surgery. This too, slowly should get better. If you notice your eye becoming so sensitive to light that you feel like covering it, this may be an indication of graft rejection.
Vision changes
Your vision most likely will improve gradually after surgery. Make a habit of checking your vision every day. Check it at the same time and in the same light. Pick an object in your house that has some pattern or detail to it – look at the object with your operated eye while covering the other eye with your hand. If your vision seems to be getting worse, this may be an indication of graft rejection.
Pain
It is normal to have occasional small twinges of pain in your eye after your operation. If your eye develops constant pain or dull aching that lasts several hours, this may be an indication of graft rejection.
Other problems that may occur
Wound separation - A small gap may ooccur in the area where the edge of the graft is sewn into the eye. You may have no symptoms at all, or you may feel a dull ache. The wound separation might be treated with a light patch or soft contact lens. It is possible the graft may require additional suturing in the operation room. Loose or broken suture – Occasionally, a suture can loosen or break during the healing process. This can cause a “gritty” foreign body sensation, especially when you blink. The loose suture can be removed easily in clinic.
Astigmatism – This occurs when the grafted cornea has the oblong shape of a football rather than the round shape of a basketball. All grafts have some astigmatism, and this usually can be corrected with glasses or contact lenses. If the astigmatism is severe a special kind of surgery often can correct it.
Frequently asked questions
How long will the surgery take?
You will be at the hospital for 4-6 hours and in the operating room for 1-2 hours.
Will I have discomfort?
Following surgery, your eye will most likely be red, irritated, and sensitive to light. You may experience increased tearing and a slight discharge. Discomfort is usually controlled with paracetamol during the first few days after surgery.
Will my eye be covered?
Your eye will be covered with a patch and a plastic shield the day of surgery. Your glasses may not fit over the patch and shield. Your surgeon / the clinic nurses will most likely remove the patch and shield at your follow up appointment the next morning after your surgery. You must wear the patch and shield over your eye while sleeping or showering.
Do I need to restrict my activities?
Your nurse and surgeon will talk to you about activity restrictions. You should avoid any activities that could involve a direct blow to the eye such as contact or ball sports.
If you live outside of the Brisbane area, it is important to stay close (within 30 minutes 1 hour) of the hospital in which you had your surgery for at least a week, as the graft will be closely monitored by the doctors during this time.
What are the potential risks of corneal transplant surgery?
All surgical procedures have risks. However, if your eye surgeon recommends a procedure, they believe the potential benefits far outweigh the potential risks. Risk of this procedure include but are not limited to the following:
| Infection of the eye | This could cause loss of vision and requires treatment with antibiotics. |
| Droopy eyelid | This may alter your appearance and can be disfiguring. Further treatment may be required. |
| Graft rejection/failure | This will require further treatment or surgery. |
| Graft detachment/dislocation | This may require a re-bubbling of the gas holding the graft in place, performed in clinic or theatre. |
| Glaucoma | An increase in pressure in the eye. This may require further treatment. |
| Bleeding | Bleeding inside the eye can occur which may need further treatment. |
| Refractive errors | You may need glasses or contact lenses after surgery. |
| Cataracts | Clouding of the lens inside the eye. This may require further surgery. |
| Sympathetic ophthalmia | Inflammation in the non-operated eye which can affect its vision. |
| Chronic pain | Can occur in rare cases, may require prescription pain relief medication. |
| Loss of vision | The vision in the eye could worsen irreversibly. |
| Loss of the eye | Can occur in rare cases |
| Contact information For any questions regarding your upcoming eye surgery, please contact the hospital via the following numbers, available Monday – Friday 8am – 4:30pm | Mater Bookings Office (07) 3163 8444 Admin team for questions regarding your booking date, time, transport, updating details. Eye Surgery Scheduler (07) 3163 8155 Nursing team regarding pre-surgery instructions for medications, fasting instructions, health and conditions. Mater Call Centre (07) 3163 3000 Regarding pre-op or post-op clinic appointments, or concerns after surgery |