Childbirth is a wonderful experience for mothers, fathers, support partners and families. Sometimes though it can result in some ongoing issues for the mum and one of these is perineal tearing—tearing of the area between the vagina and anus. These tears can range from being small abrasions to deep lacerations that affect the pelvic floor muscles. Most often, though a tear will simply be an abrasion needing to be stitched and will heal well. But some tears are worse than others and affect the pelvic floor muscles which can affect a mother’s broader health sometimes even having a lifelong impact on physical, psychological & social health and wellbeing.
The Women’s Healthcare Australasia (WHA) has worked collaboratively with Mater Mothers’ Hospitals and several other Australian maternity hospitals to develop ways to avoid or minimize a third or fourth degree tear from occurring. The collaboration is committed to reducing the harm caused by third and fourth degree tears because while only 4% of women sustain a third or fourth degree tear they can have continuing bowel, bladder and sexual problems for varying amounts of time but sometimes even permanently. These lasting effects can be minimised with timely, accurate diagnosis and follow up.
What are perineal tears?
- Perineal tears affect the skin and muscles of your perineum, between your vagina and anus
- First and second degree tears are quite common and usually heal without difficulty
- These tears may need stitches and follow up with your local doctor.
What are third and fourth degree tears?
- Third degree tears go through the muscles that control the anus (back passage)
- Fourth degree tears extend into the lining of the anus or rectum. Third and fourth degree tears usually require repair in an operating theatre.
Could this happen to me?
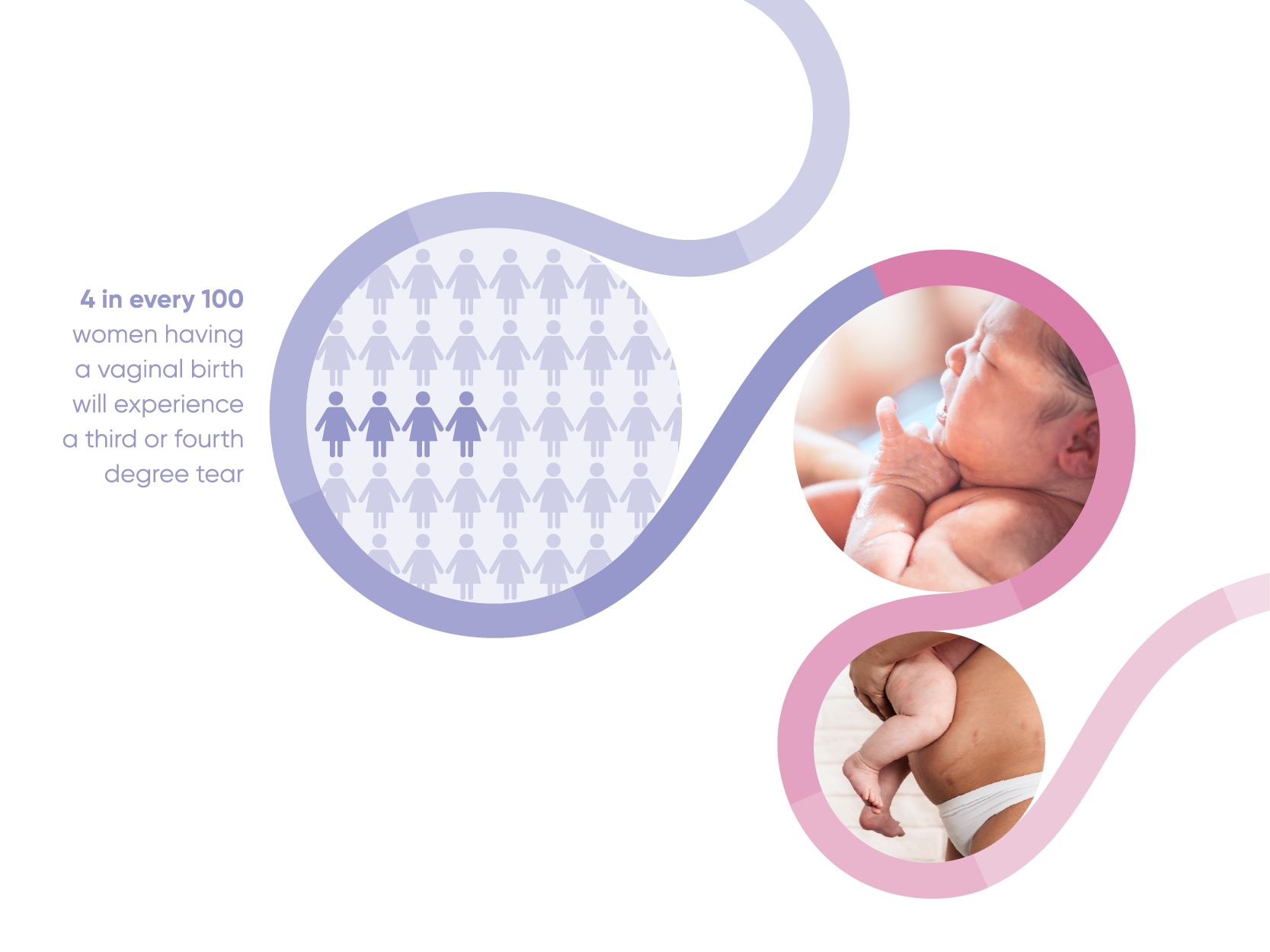
Approximately 4 out of every 100 women having a vaginal birth experience a third or fourth degree tear.
Your chance of a third or fourth degree tear is increased if:
- This is your first baby
- You are of Southeast Asian background
- You have previously had a third or fourth degree perineal tear
- Your baby weighs more than 4kg (9lb) or is in a position with their back against your back (posterior)
- Your baby’s shoulders become stuck during birth
- You require forceps or other instruments to assist your birth.
What does this mean for my care?
As part of our commitment to reducing avoidable third and fourth degree tears, women having vaginal births will be offered the following care:
- Application of a warm washcloth (compress) to your perineum when your baby’s head is crowning. This helps the muscles in your perineum stretch naturally
- Encouraging you to move and to adopt birthing positions that control your birth during the second stage of your labour (e. g. on hands and knees)
- Helping you to have a slow, controlled birth through breathing techniques, and without directed pushing
- Using hands to gently support your perineum during the birth of your baby’s head.
For births that require instrumental assistance
Sometimes instruments, such as forceps or a vacuum (Ventouse) are needed to assist with the birth of your baby. Forceps and Ventouse are instruments that enable your obstetrician to pull, in time with your contractions, to assist with the birth of your baby.
Which instrument is used depends on how your birth is progressing and the position your baby is in. These instruments can help the mother and baby achieve a safe vaginal birth.
If this is your first birth and you require assistance by forceps or Ventouse we will recommend an episiotomy. An episiotomy is a cut made with scissors at the entrance to your vagina into the perineum.
An episiotomy can help to reduce third and fourth degree perineal tears. We will ask for your permission to cut an episiotomy and pain relief will be provided.
How will I know if I have a third or fourth degree perineal tear?
After the birth of your baby we will examine your perineal and anal area to see if you have a perineal tear. To ensure a tear is not missed we recommend a rectal examination for all women.
This examination can detect internal tears, and ensures we are able to offer appropriate treatment and follow up.
We will ask for your consent before we conduct this examination, and you can withdraw your consent for the examination at any time.
At the very end of your labour the skin and muscles around your vagina thin and stretch to allow your baby to be born. It is quite common for women to have some form of perineal or vaginal tearing.
Caring for your perineum after birth
- Keep your perineum clean and free from infection
- Wash your perineal area several times a day and after each bowel motion.
- Change your sanitary pads every four to six hours.
- Always wipe (or pat) from front to back after going to the toilet.
- Do not use a hairdryer to dry your perineum—this may delay healing or cause burning to the area.
- Avoid the use of creams, ointments or powder.
- Antibiotics may be prescribed by your doctor to prevent wound infection
Keep comfortable
- Apply ice packs to the area every couple of hours for at least 24 to 48 hours.
- Take regular pain relieving medication as prescribed by your doctor.
- Lie down to rest for 20 to 40 minutes each hour as this will help the area to heal.
- When feeding your baby shift your sitting position or feed lying down.
- Get in and out of bed on your side as this reduces any strain to your perineum
Emptying your bowels
For the first few days a low fibre diet is recommended to prevent any further damage to your perineum due to straining to pass a bowel motion. At the same time you will be given a softening agent such as Lactulose to ensure soft bowel motions. Drink eight glasses of water per day.
Make sure you try not to strain when using your bowels and use the recommended defaecation position. The passage of hard stools can disrupt repair and delay healing. Support the perineum with your hand while emptying your bowels, laughing, coughing, etc.
After three days you will need to eat a high fibre diet to assist with the passage of soft, easily expelled bowel motions. If you are usually prone to constipation please talk to your doctor about appropriate management—using softening agents for up to six weeks after the repair may assist your recovery.
Postnatal exercises
Your physiotherapist will teach you how to do gentle pelvic floor contractions to assist healing, improve circulation and decrease swelling and pain. You will also learn how to use your muscles to protect your perineum before and as you move. This is important for early recovery and functional protection of sutures. We recommend you avoid excessively strong pelvic floor exercises for six weeks after the birth of your baby. Gradually increase the strength of contraction/length of hold/number of repetitions of your pelvic floor exercises over the first six weeks after the birth of your baby.
Going home
Your doctor will be able to advise you when you are ready for discharge so ensure that you discuss any concerns you may have at this time. It is also very important that you continue to look after your perineum when you go home.
Follow up care
It is important that you attend all your follow up appointments so that your recovery can be assessed.
One to two weeks
A Mater physiotherapist will contact you to ask you about your recovery.
Six weeks
Physiotherapy appointment—you will be given an appointment to see a physiotherapist, who specialises in pelvic floor function, to check your progress and review your longer-term strengthening program.
Check-up with your family doctor (GP)—please make an appointment to see your GP for a check-up six weeks after the birth of your baby, as part of your routine postnatal care. Contact your GP earlier if you have any concerns about your recovery.
Three months
You will receive a follow-up phone call from the postnatal clinic at three months. A face-to-face appointment will be arranged if:
- any issues are identified by the physiotherapist during follow up
- you would prefer a face-to-face appointment
- your situation is not appropriate for phone follow up (e.g. you require an interpreter)
- any issues are identified during the phone consultation.
Frequently Asked Questions
When can I resume sexual activity?
Comfortable sexual activity can begin after your body has completely healed which may take from six weeks to several months. If you experience ongoing discomfort during sexual intercourse it is important that you discuss this with your doctor.
When can I go swimming?
When your bleeding has stopped and your stitches have healed.
What about future births?
Advice about future births will depend on how well you recover from this one. If you are fully recovered there at the time of your next pregnancy there is little evidence to suggest the best way for your baby to be born. However if you have some ongoing incontinence problems, especially with your bowel, a vaginal birth may make this worse. When you are seen in the Perineal Clinic, (via a telephone call or face-to-face appointment), the doctor will discuss with you the most appropriate way for your next baby to be born, depending on your individual situation.
If you have any further questions about what happened this time, please ask to speak to your doctors prior to going home.