Treatment
Our gynaecological oncology service cares for both private and public patients, providing advanced treatment with a focus on minimally invasive techniques including laparoscopic and robotic surgery. These approaches can support faster recovery, minimise pain, and improve outcomes for women.
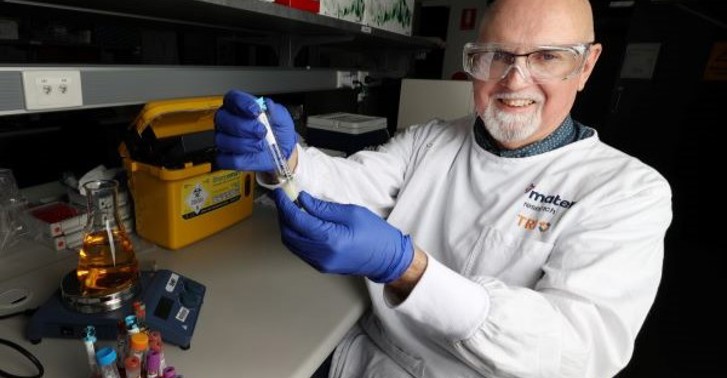
We work closely with Mater Research and the Queensland Centre for Gynaecological Cancer Research (QCGC Research), contributing to more than 20 national and international research projects that are shaping the future of gynaecological cancer care.
Mater is also one of the few centres in Australia trialling Hyperthermic Intraperitoneal Chemotherapy (HIPEC) for ovarian cancer—a promising treatment showing improved survival outcomes. As evidence grows, HIPEC is expected to become more widely available across gynaecological oncology units nationwide.